Understanding Stress Incontinence and Solutions
Imagine this: you are trying to lose weight, and you are excited that you joined a local gym with classes that are included with your membership. You walk into your first HIIT class, and realize about halfway into the class, that there is a lot more jumping than you were prepared for, and you are slowly starting to feel more and more leaking as the class goes on.
You can hear your gynecologist’s voice in the back of your mind…”Just do you kegels!” These experts often blame the pelvic floor. You’ve had one, two, three babies? Maybe more? Your pelvic floor has been stretched out! You just need to squeeze as hard as you can to make it stronger. If you don’t you will be left wearing pads and panty liners the rest of your life, possibly with a surgery to repair your bladder prolapse down the road.
But is there more to this story? Could it be that your pelvic floor muscles are weak, but it’s not just from having a baby or two? Could there actually be another way that doesn’t involve thousands and thousands of kegels?
In this blog, we’ll dive deep into the science, challenge the myths, and reveal whether kegels are truly the answers to solving incontinence - or if there is more to the story of strengthening your pelvic floor to prevent stress incontinence.
The role of your pelvic floor
Before we get into the nitty gritty of how to solve stress incontinence, we need to take a deeper look at WHAT the pelvic floor is, and how it is designed to function.
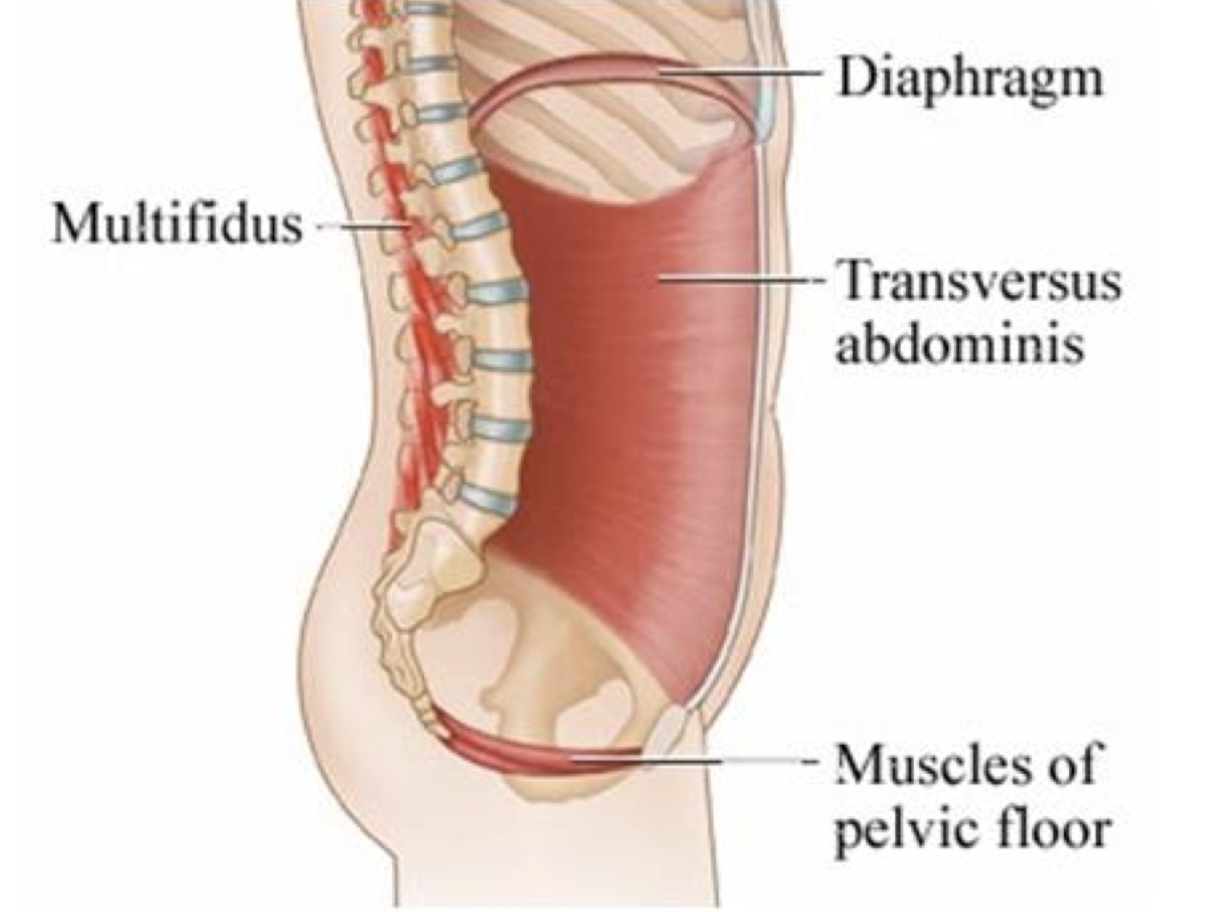
The pelvic floor is a group of tendons, muscles and ligaments that attach to your pubic symphysis in the front, your coccyx (or tailbone) in the back, and then your sit bones out to the sides. There are multiple layers of these muscles, and they are all connected by tissue called fascia to work together as a unit to provide the support your body needs.
But let’s get more specific. What do these muscles actually do?
Support: these muscles help to support all of the organs that sit inside of your pelvis. This would include your bladder, uterus and rectum.
2. Stability: these muscles are a part of your core, meaning they work WITH your abdominal muscles, your diaphragm, and some spinal muscles called your multifidus to create a stable base for the rest of your body.
3. Sexual: orgasm, erection, and ejaculation are results of pelvic floor function. So that thought that maybe you would have a stronger orgasm if your pelvic floor was functioning properly? Not a myth!
4. Sphincteric: we need these muscles to keep things in when we need them to stay in (like when we are taking a HIIT class at the gym), but we also need them to relax and lengthen and soften when we are ready to let things come out.
So how does all of this start to apply to leaking with a jumping jack? Well, let’s take our hammock analogy a step further, and consider instead a trampoline.
The black mesh in the center of the trampoline is comparable to your pelvic floor muscles. If that black mesh is not tight enough, we might need to say a prayer that it will hold you up when you jump on it! Same for your pelvic floor muscles, there needs to be an adequate amount of integrity and strength to these muscles so that it can hold up any kind of pressure applied (sneeze, laugh, cough, etc.)
BUT, let’s imagine that whoever assembled our trampoline was a little too ambitious and tightened that black mesh part way too much. When you take your first bounce on it, OUCH! There is no give at all, and that probably didn’t feel good for your body or the trampoline itself. Your pelvic floor muscles need to relax, lengthen and soften in order to adequately absorb shock, force and pressure that is applied. So that jumping jack? Let’s make sure your muscles can accept an increased load and pressure first.
So, what causes stress incontinence?
Stress incontinence is defined as any action or movement that causes an increase in intra abdominal pressure (coughing, sneezing, laughing, jumping, running), where your pelvic floor muscles can then not withstand the increase in pressure, and thus leaking happens. There are several factors that can contribute to the development of stress urinary incontinence in women. Let’s dive into a few.
Weak and Over Lengthened Pelvic Floor Muscles
It is true that there is a correlation between vaginal births and stress urinary incontinence. One study compared women who gave birth vaginally to those who had a cesarean birth, and found that women with a history of vaginal births were more likely to develop stress urinary incontinence (1). However, what’s important to note is that even though the women with vaginal births were MORE likely to develop incontinence, women with cesarean births could still develop incontinence.
Why is this?
Pregnancy takes a toll on our bodies and pelvic floors. These muscles have to accomodate for an increase in pressure and load for 40 weeks. That’s a long time! And can you imagine what it would be like for these muscles to do this multiple times?!
If there is no rehabilitation or strengthening for these muscles postpartum, there could be dysfunction that happens down the road.
Restricted Pelvic Floor Muscles
Let’s pause and consider the trampoline again. If that trampoline is too taught, and you jump on it over and over and over again, there is going to be damage done to the trampoline because it isn’t functioning how it was designed to.
Your pelvic floor muscles were designed to absorb shock. Just like any other muscle in our body is designed to absorb shock. If we are adding pressure and stress to muscles that are tight, rigid, shortened, they are going to become weaker over time. They are not given a chance to fully relax and work through their full range of motion.
Let’s think about a muscle that is easiest to visualize, like your biceps. If your elbow is bent, your biceps are shortened. Now, let’s say you cannot extend your elbow all the way to get it completely straight, so you are just doing bicep curls over and over again with your elbow already halfway bent. Are you strengthening your biceps in an efficient way? No! Will this make your biceps stronger? Probably not! In fact, you might even be making it weaker by not strengthening it through it’s full range of motion.
Same thing with your pelvic floor muscles. We have to be able to fully lengthen and fully contract these muscles. If we are not fully lengthening and relaxing our pelvic floor muscles, we are likely making them weaker over time.
Decreased Estrogen
A lot of women will notice that their incontinence worsens as they get older. Why?
During menopause, there is a decrease in estrogen. This can lead to a decreased amount of tone in the pelvic floor muscles, which can then lead to more weakness and decreased function (2).
Postpartum can also be a period of time in a woman’s life where she experiences a decrease in estrogen levels, particularly if she is breastfeeding. There will be a sharp drop in estrogen due to the increase in prolactin which is needed for producing breast milk. This can also lead to similar symptoms of dryness and decreased tone of the pelvic floor muscles.
The graph below is a rough depiction of how the levels of estrogen change throughout a woman’s lifespan.
Poor Bladder Hygiene and Habits
Your pelvic floor muscles are meant to fully relax and lengthen to allow urine to exit the bladder. Many women will go to the bathroom when they first feel the urge to urinate, even though the bladder is not all the way full.
If you are emptying your bladder frequently, before your bladder is completely full, the pelvic floor muscles are not able to be stressed to support a full bladder. If these muscles are not having to support a full bladder consistently, then can become weaker over time.
Poor Coordination
Your pelvic floor muscles work with the rest of the your body to do their job in providing stability. If your pelvic floor muscles are overworking, or underworking, they are not properly coordinating with the rest of your core to provide that stability. We need everything working optimally together to provide the maximum amount of support and stability so that you can do that jumping jack without peeing.
This same concept applies to the other parts of your body that impact your pelvic floor. How are your hips moving? How are your ankles? Do you have low back pain? Nagging hip pain that won’t go away? Oftentimes all of these issues are connected, and all need to be addressed in order to solve the problem of incontinence.
One study found that pelvic floor muscles produced a stronger contraction when there was an increase in ankle dorsiflexion (3). If your ankles are stiff, this is going to impact how your pelvic floor muscles are functioning. We cannot ignore the rest of our body, but must consider how our different body parts and muscles influence each other.
The Problem with Kegels
Put simply, your pelvic floor muscles do not work in isolation. Your pelvic floor muscles were designed to function alongside the rest of the muscles in your body, against gravity. I don’t know about you, but I very rarely spend time on my back throughout the day.
I’m working, picking up my baby, going for runs, and functioning on my feet, against gravity! So shouldn’t our pelvic floor be challenged to support us in this way?
Is there a time and a place for kegels? You bet. Is this the only solution to strengthening your pelvic floor? Nope. And if anyone tells you differently, run the other way!
So Where Do We Go From Here?
Bottom line, we need to be able to fully relax and fully contract our pelvic floor muscles in a variety of contexts and exercises so that when we cough or sneeze, our muscles have the strength to withstand that increase in pressure.
Here are 5 of my favorite exercises to engage the pelvic floor muscles, and to make sure they are able to do both.
2.TA activation with PF contraction with pillow under hips
1.Tsui, W.L., Deng, GH., Hsieh, TC. et al. Association between vaginal or cesarean delivery and later development of stress urinary incontinence or pelvic organ prolapse: A retrospective population-based cohort study. Int Urogynecol J 34, 2041–2047 (2023). https://doi.org/10.1007/s00192-023-05504-62.Ayten, D. İ. N. Ç. (2019). Menopause and Urinary Incontinence. Recent Studies in Health Sciences, 341.
3.Kannan P, Winser S, Goonetilleke R, Cheing G. Ankle positions potentially facilitating greater maximal contraction of pelvic floor muscles: a systematic review and meta-analysis. Disabil Rehabil. 2019 Oct;41(21):2483-2491. doi: 10.1080/09638288.2018.1468934. Epub 2018 May 7. PMID: 29733699.